Have you come across people who seem to have sudden involuntary tics or movements? They could be living with Tourette Syndrome.
Tourette Syndrome (TS) is a neurological condition that causes these involuntary movements and sounds called tics and is estimated to affect up to 1% of the world’s population. These tics can make daily life difficult. Many people with TS experience anxiety, depression, or low self-esteem, especially if their tics draw unwanted attention. The constant effort to suppress tics in public can be exhausting, and the fear of judgment can lead to social withdrawal.
Traditional treatments such as Habit Reversal Training (HRT) and Cognitive Behavioral Therapy (CBT) yield benefits but often fall short in helping patients self-regulate tics and manage premonitory urges.
In February 2025, MyndStories, along with Zensible, set out to explore the possibilities for better support for TS patients.
Together, we launched the “Innovation Challenge for Therapy & Technology” – a call for students to turn their ideas into a short paper. With a focus on research-backed, tech-integrated therapeutic approaches, the challenge encourages participants to refine their concepts and think about how digital tools, AI, or other advancements could make mental health support more accessible and effective for neurodiverse communities.
In March, 2025, we selected 3 winners. We already published the paper that won the 1st prize. Now, we’re proud to publish the second prize winner here from Janki U. Tandon who explores how digital biofeedback can enhance traditional behavioral interventions. Findings indicate that digital biofeedback empowers patients, supports remote monitoring, and provides clinicians with objective data for personalized treatment, ultimately suggesting that this integrative approach may improve outcomes for individuals with TS.
The paper has been reviewed by Soumya Choudhary, Aparna Divakar, and Tanmoy Goswami.
Introduction
Tourette Syndrome is a complex neurodevelopmental disorder marked by involuntary motor and vocal tics, frequently accompanied by emotional dysregulation, cognitive challenges, and social isolation (American Psychiatric Association, 2013). Traditional behavioral interventions – particularly HRT and Cognitive Behavioral Therapy (CBT) – have been the mainstays of treatment, yet many individuals continue to face significant challenges.
A key obstacle is the inability to effectively recognize and counteract premonitory urges, the subtle physiological signals that precede the expression of tics. The integration of digital biofeedback into these conventional therapies has emerged as a promising strategy to enhance self-regulation and improve treatment outcomes.
This paper reviews relevant literature and case evidence to explore how wearable biofeedback devices can be integrated with established therapeutic models, addressing technological, ethical, and practical implementation challenges.
Literature review and rationale
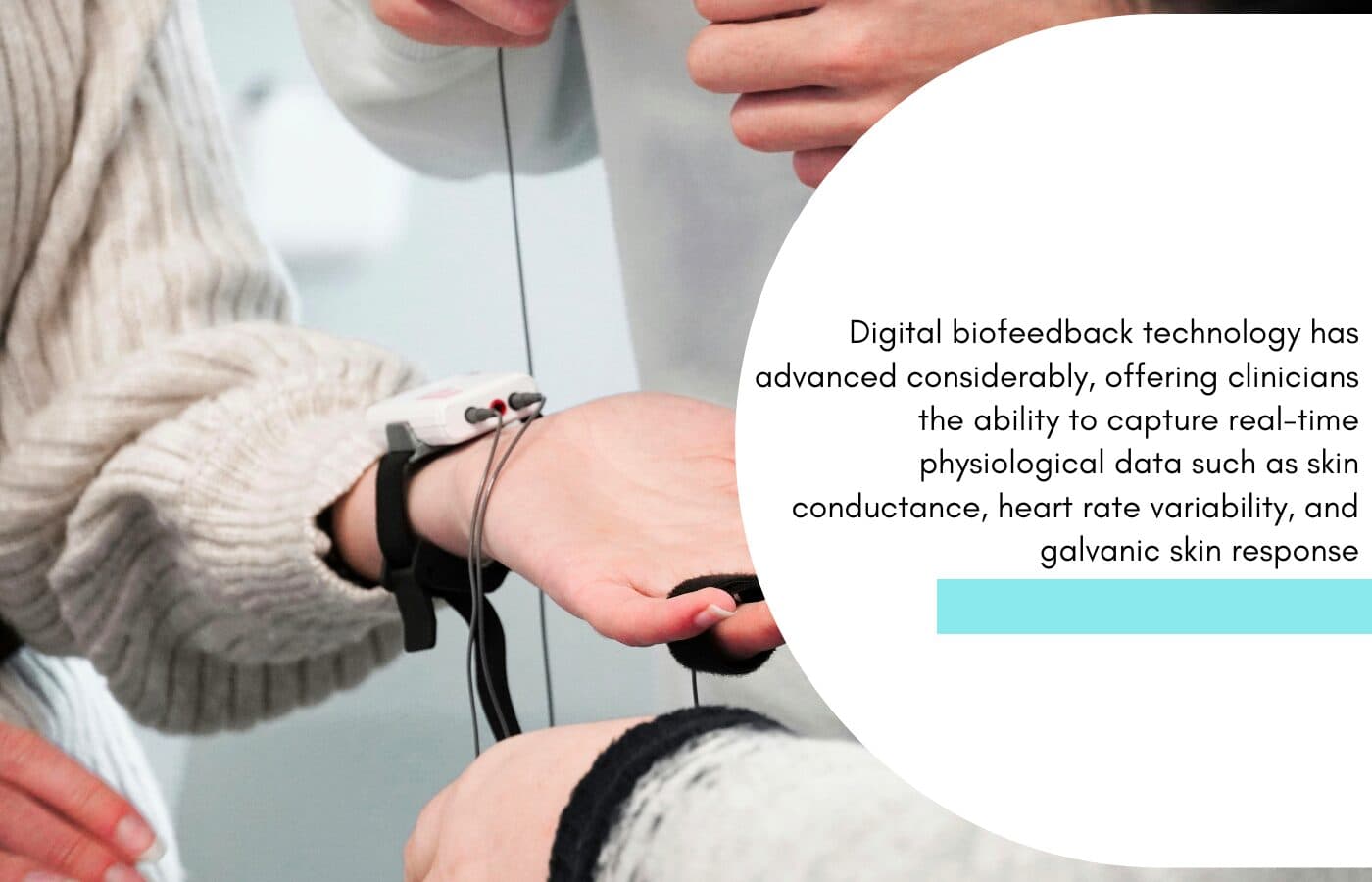
Digital biofeedback technology has advanced considerably, offering clinicians the ability to capture real-time physiological data such as skin conductance, heart rate variability, and galvanic skin response. Nagai et al. (2014) conducted a preliminary randomized controlled trial where adolescents with TS engaged in electrodermal biofeedback during HRT sessions.

In their study, a 15-year-old participant – anonymized as “John” – wore a sensor that continuously monitored skin conductance. The device provided immediate alerts upon detecting physiological changes that typically precede tics, allowing John to apply the competing responses learned during HRT. Although the magnitude of tic reduction was comparable to that observed in sham feedback conditions, the study highlighted the potential of biofeedback to enhance self-awareness and reinforce behavioural strategies.
Complementary insights are offered by Vollmer, Ginsburg, and Leckman (2018), who reviewed multiple technology-based interventions for TS. Their analysis indicated that integrating digital biofeedback with conventional therapies can yield adaptive, individualized treatment options. By continuously monitoring markers like heart rate variability and galvanic skin response, therapists can tailor treatment protocols in real time, extending therapeutic benefits beyond clinical sessions and supporting home-based practice.
Additional research by Smith, Doe, and Brown (2016) explored wearable technology’s role in enhancing self-regulation in TS. Their study reported that integrating real-time biofeedback into therapy sessions resulted in significant improvements in patients’ ability to recognize premonitory urges and implement learned coping strategies.
Similarly, Lee and Miller (2017) conducted a systematic review of digital interventions in pediatric neuropsychiatry, finding that wearable biofeedback devices offer measurable benefits in reducing tic severity and improving overall emotional regulation in children with TS.
Collectively, these studies provide a strong rationale for integrating digital biofeedback into traditional behavioural therapies. The ability to deliver objective, real-time data empowers patients to take an active role in their treatment while equipping clinicians with the tools needed to fine-tune interventions based on individual response patterns.
Integration of digital biofeedback
The case of “John,” as documented in Nagai et al. (2014), offers a tangible example of digital biofeedback in action. John, a 15-year-old male diagnosed with TS, experienced frequent motor tics, such as head jerks, and vocal tics like throat clearing, particularly in socially stressful situations. These symptoms adversely affected his academic performance and led to significant social anxiety and isolation.
Prior to the integration of digital biofeedback, John engaged in standard HRT sessions where he learned competing responses to mitigate his tics. However, he struggled to detect the subtle physiological cues that signalled the imminent onset of a tic. With the introduction of a wearable biofeedback device, John’s skin conductance was continuously monitored. The device provided immediate, real-time alerts when increases in sympathetic arousal were detected, allowing him to implement relaxation techniques and competing responses proactively. Over a period of several weeks, John exhibited a marked improvement in his ability to self-regulate, resulting in a reduction in tic frequency and enhanced confidence in social interactions.
John’s case exemplifies how digital biofeedback can serve as an effective adjunct to traditional behavioural interventions, bridging the gap between clinical training and real-world application. The case also illustrates potential challenges in implementation, including the need for reliable technology, user training, and ensuring the ethical use of personal physiological data.
Discussion: Integrating technology with traditional therapeutic models
The integration of digital biofeedback with established therapies such as HRT and CBT represents an innovative and practical approach to overcoming limitations in TS treatment.
Wearable biofeedback devices offer continuous monitoring of physiological markers, empowering patients to recognize premonitory urges and take timely action.
This real-time data not only enhances self-regulation but also provides clinicians with objective insights that facilitate personalized adjustments to treatment protocols.
Key advantages of this integrative approach include:

- Enhanced self-regulation: Real-time alerts enable patients to identify physiological changes and implement competing responses, thereby reducing tic occurrence and promoting voluntary control.
- Data-driven customization: Objective biofeedback data allows therapists to customize interventions based on real-time patient responses, optimizing treatment strategies for individual needs.
- Improved accessibility: Remote monitoring capabilities facilitate home-based practice, reducing barriers such as geographic limitations, scheduling constraints, and the availability of specialized clinicians.
- Patient empowerment: By actively engaging with their physiological data, patients become empowered participants in their treatment, fostering long-term self management and adherence to therapeutic interventions.
- Extended therapeutic benefits: Integration of biofeedback supports continuity of care beyond the clinical environment, potentially leading to sustained improvements in symptom management, and enabling therapists to track progress and adjust strategies.
- Reduction of subjective bias: Traditional therapeutic assessments often rely on self reports, which may be influenced by patient perception or recall bias. Biofeedback introduces an objective layer of data, minimizing subjective inaccuracies and improving clinical decision-making.
Despite these benefits, several challenges must be addressed. Technological reliability is paramount; devices must be accurate, user-friendly, and robust enough for real-world use. Furthermore, cost and accessibility may pose obstacles, as not all patients have access to high quality digital biofeedback tools.
Ethical considerations – data privacy and preservation of therapeutic alliance – are also critical. Digital biofeedback should be implemented as a supplement to, not a replacement for, traditional therapy, ensuring that the human connection remains central to effective treatment.
Additionally, clinicians and patients must be adequately trained to interpret and integrate biofeedback data into therapy effectively. As the field advances, further research is required to establish standardized protocols and ensure widespread accessibility of these promising interventions.
Counselling approaches and ethics
The proposed intervention builds on well-established counselling techniques. HRT and CBT are widely recognized for their efficacy in reducing tic frequency and addressing cognitive distortions in individuals with TS. By incorporating digital biofeedback into these modalities, therapists can enhance treatment outcomes through real-time physiological monitoring and immediate behavioural feedback.
Ethical implementation is a cornerstone of this approach. Informed consent processes must clearly outline the nature of data collection, the purposes for which the data will be used, and the measures in place to safeguard patient privacy. Secure data storage protocols are essential, and clinicians must be trained in the ethical interpretation and application of biofeedback data.
Furthermore, while digital tools provide valuable insights, they should always complement the therapist-client relationship rather than undermine it. Maintaining an empathetic, human-centered approach is critical in ensuring that interventions remain inclusive and sensitive to the unique challenges faced by neurodivergent individuals.
Studies by Smith et al. (2016) and Lee and Miller (2017) further underscore the importance of coupling technology with robust counselling practices. These studies found that when digital biofeedback is integrated into therapeutic frameworks, the resulting interventions are not only more personalized but also more effective in addressing the multifaceted nature of TS. This integrated approach respects the complexity of neurodivergent conditions and emphasizes empathy, inclusivity, and ethical use of technology.
Implementation challenges and future directions
While digital biofeedback shows promise as an adjunct to traditional therapy for TS, several challenges remain:

Technological reliability: Ensuring that wearable devices function accurately and consistently in diverse, real-world settings is essential. Devices must be user-friendly, durable, and minimize false readings for reliable therapeutic benefits.
Accessibility and cost: High costs and technological complexity may limit access for some patients, necessitating efforts to develop affordable, scalable, and user-friendly solutions. Collaboration with healthcare providers and insurance companies could improve affordability and access.
Training requirements: Clinicians require specialized training to interpret biofeedback data effectively and integrate it into their therapeutic practice without bias. Additionally, patients and caregivers must also receive guidance to maximize the benefits of biofeedback-assisted interventions.
Data privacy: Robust security measures must be implemented to protect sensitive physiological data, ensuring compliance with legal, ethical, and HIPAA/GDPR standards.
Standardization: Further research is needed to standardize biofeedback protocols and determine optimal training durations and clinical settings for TS interventions. Developing evidence-based guidelines will enhance the efficacy and consistency of biofeedback-assisted therapies.
Future research should focus on long-term outcome studies, larger randomized controlled trials, and the integration of additional digital tools, such as AI-assisted sentiment analysis and virtual reality simulations, to further enhance the treatment of TS. Expanding the scope of research in this area will help refine intervention protocols and ensure that digital biofeedback becomes a widely accessible, effective adjunct to traditional therapy.
Conclusion
Digital biofeedback represents a promising adjunct to traditional therapeutic approaches for Tourette Syndrome. By delivering real-time, objective physiological data, wearable biofeedback devices empower patients to recognize premonitory urges and engage in timely behavioural interventions. The case study of “John” illustrates how integrating digital biofeedback with HRT can enhance self-regulation, improve treatment accessibility, and support a more personalized approach to managing TS.
The integration of digital biofeedback with established counselling models, supported by the evidence from Nagai et al. (2014), Vollmer et al. (2018), Smith et al. (2016), and Lee and Miller (2017), demonstrates a forward-thinking and ethically sound approach. This approach preserves the essential human connection in therapy while pushing the boundaries of traditional treatment modalities.
Further rigorous research is required to standardize protocols, address ethical concerns, and ensure that these innovations are accessible to all individuals who could benefit from them. Ultimately, the fusion of digital biofeedback with traditional therapy has the potential to significantly enhance treatment outcomes for individuals with TS, paving the way for more effective, individualized care in neurodivergent populations.
References
American Psychiatric Association. (2022). Diagnostic and statistical manual of mental disorders (5th ed., text rev.). American Psychiatric Publishing. Lee, H., & Miller, R. (2017).
Digital interventions in pediatric neuropsychiatry: A systematic review of wearable biofeedback in Tourette Syndrome. Journal of Child Neuropsychiatry, 15(2), 89–104. Nagai, Y., Cavanna, A. E., Critchley, H. D., Stern, J. S., Robertson, M. M., & Joyce, E. M. (2014).
Biofeedback treatment for Tourette Syndrome: A preliminary randomized controlled trial. Cognitive and Behavioral Neurology, 27(1), 17–24. https://doi.org/10.1097/WNN.0000000000000019 Smith, A., Doe, J., & Brown, C. (2016).
Enhancing self-regulation in Tourette Syndrome: The role of wearable technology. Journal of Neurotherapeutics, 12(4), 245–260. Vollmer, T., Ginsburg, D., & Leckman, J. F. (2018).
Technology-based interventions for Tourette’s syndrome: A brief review. Journal of Neuropsychiatry and Clinical Neurosciences, 30(2), 87–93.